Shortness of breath and respiratory distress are very unpleasant. The feeling of not getting any air, or too little air, can have different causes. If you have regular or permanent shortness of breath, you should see your doctor to investigate why.

There are many reasons respiratory distress may occur. We need to distinguish between acute respiratory distress, which can be an emergency - for example, in asthmatics, where an emergency doctor may have to be called - and shortness of breath, which occurs when the bronchial tubes are already constricted, and increases under stress, such as in COPD patients.
Overview – possible causes of shortness of breath:
If you experience shortness of breath associated with a respiratory disease, this is usually caused by the mucous membrane in the bronchial tubes swelling (due to allergies or inflammation). This leaves the bronchi unstable, so they can collapse, which then narrows the inside space (lumen) through which air can flow in and out. The bronchial tubes then feel tight and it is more difficult to breathe. Another cause of respiratory distress can be cramping of the respiratory muscles, which very quickly narrows the airways.
Shortness of breath and respiratory distress can occur or become worse in certain situations. Examples for this are:
The more sensitive the lungs, the more they react to external irritants. You may, for example, find that a few weeks after a serious lung infection you become short of breath and have to cough if you are standing by a campfire or open fire, even if that never gave you breathing problems before.
Heads up: You should call an emergency doctor if the respiratory distress is acute and is deteriorating. Asthmatics should make sure they always have their emergency medication on them.
For shortness of breath that does not pose an acute threat, try these three tips. You can also use these prophylactically.
Monitor yourself. What causes shortness of breath? Can you avoid these situations? Yes? Then do so!

Calm your breathing and do the exercises that help your airways and breathing relax.
For instance:
Breathing relief by relieving the weight of your arms. Place your arms on a railing, for example, or adopt a goalkeeper position. Click here for instructions on exercises that relieve strain and other exercises to counteract respiratory distress and panic attacks.
Pursed lip breathing: Pursed lip breathing involves breathing calmly and evenly through slightly pursed lips. Pursed lip breathing is a form of PEP breathing.
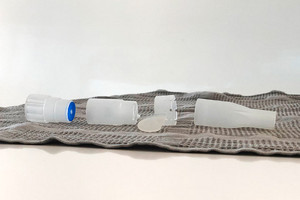
PEP breathing: PEP breathing is when you exhale against resistance. This can also be achieved with assistive devices. Examples of assistive devices of this kind are the PARI PEP S or the PARI-O-PEP. Both devices are available in the pharmacy or online.
If your shortness of breath is caused by a respiratory disorder, your doctor may prescribe you inhalation medications that expand the airways. These are inhaled either via a spray or metered dose inhaler or an inhalation therapy device. Ask your doctor to explain these to you.
A holding chamber makes the metered dose inhaler easier to use and ensures that the contents reach the lungs and do not dissipate in the mouth or throat. This risk is particularly high in patients who have permanent respiratory distress or who develop shortness of breath especially when they breathe faster. PARI offers the VORTEX holding chamber that allows you to inhale with calm and relaxed breathing with the metered dose inhaler for several breaths in hygienically safe conditions. Your doctor can prescribe you the VORTEX, although you can buy it yourself in the pharmacy or online.
You can also inhale medications that expand the airways with inhalers such as the PARI BOY CLASSIC. While inhalation therapy may take longer than inhaling with a metered dose inhaler, it does have other advantages:
PARI nebulisers are available in pharmacies and online. All models can also be prescribed by your doctor.
NOTE: The information in this article does not constitute a treatment substitute. The exercises presented should be used as examples for breathing therapy. PARI recommends that patients always consult with their physician or physiotherapist first
An article written by the PARI BLOG editorial team.
© 2025 PARI GmbH Spezialisten für effektive Inhalation