Pulmonologist Prof. Fischer takes a look at the causes of and therapies for mucus in COPD and bronchiectasis, and explains how they differ from each other – and shares some practical tips.

Stubborn mucus in the bronchial tubes is a distressing symptom for many people with COPD or bronchiectasis. We interview Munich pulmonologist Prof. Rainald Fischer who explains why this mucus develops, what the differences in mucus production are between the two diseases and the most effective ways to clear these secretions. As well as explaining the medical background, he shares practical tips for managing daily life with the condition.
Prof. Dr Fischer: The main reason for mucus production is chronic inflammation in the airways. The inflammation triggers the cells that produce the mucus to step up production. The lungs produce mucus to help transport harmful substances they identify as pathogens upward and out of the bronchial tubes along with the secretions. Mucus production is a natural reaction of the lungs to fight off infections.
This inflammation is chronic in chronic obstructive pulmonary disease (COPD) and bronchiectasis. This leads to mucus being produced all the time. With bronchiectasis, there is the added problem that bacteria such as Staphylococcus aureus or Pseudomonas aeruginosa that often lurk in these dilated bronchial tubes exacerbate the inflammation. This increases the tendency for mucus production even further.
Prof. Dr Fischer: The key difference is that in patients with bronchiectasis, the bacterial colonisation also causes more inflammation and thus mucus production. Both diseases feature underlying chronic inflammation, but in bronchiectasis, the bacteria exacerbate the situation.

Prof. Dr Fischer: Excess mucus in COPD is not a sign that it is a severe course – it is just a symptom of the disease. There are patients with “dry” COPD (although “dry” is a bit of an exaggeration), who hardly produce any mucus, and then there are others who produce a great deal. Smokers and ex-smokers in particular produce more mucus.
People who have COPD not associated with smoking, e.g. caused by particularly severe and frequent infections in childhood, often have less mucus. So mucus production with COPD is not necessarily a sign of disease severity. Nonetheless, a buildup of mucus in the bronchial tubes is unpleasant, as it makes it harder to breathe and triggers a cough.
Prof. Dr Fischer: It is important to treat the underlying disease. For COPD, there are drugs available like anticholinergics and inhalative corticosteroids. Bronchiectasis – irreversible dilatation of the bronchial tree – causes structural and irreversible changes to the lungs. Bacterial colonisation can be treated with antibiotics – orally, intravenously or, in exceptional cases, inhalative. Mucolytic or expectorant treatments can also bring about an improvement. Inhalation therapy with an inhalation device is particularly suitable and effective in this case.
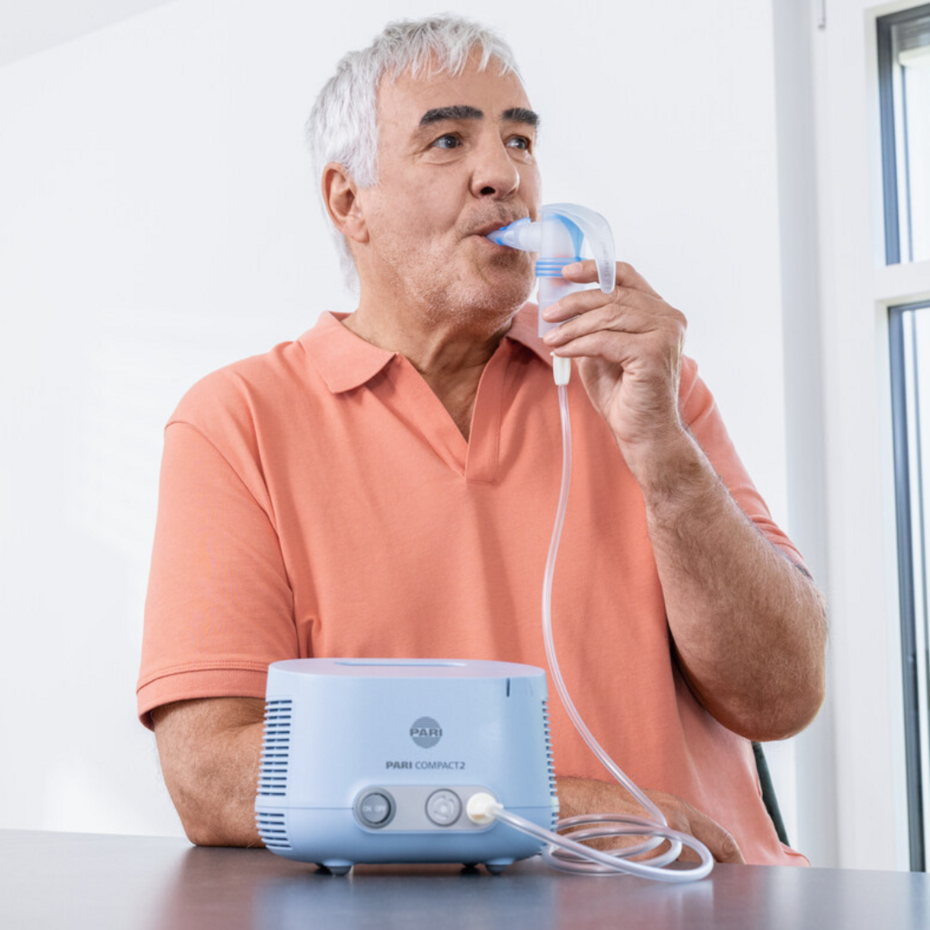
Prof. Dr Fischer: The ideal option is a 3 or 6 percent hypertonic saline solution, as it efficiently loosens mucus. Some patients find that too irritating, in which case a 0.9 percent saline solution can be used for the inhalation therapy. NaCl 0.9% does not explicitly have an expectorant effect, but moistening the bronchial mucous membranes and the secretions still helps mobilise the mucus out of the lungs so it can be coughed up. This is what patients report all the time. In this case it is important that the inhalation solution is inhaled with an inhalation device so that the droplets are respirable and can reach the bronchial tubes.
Inhaling saline solutions over hot steam has no effect – not only for loosening mucus in COPD and bronchiectasis, but in general as well. It is a prevailing myth, even though steam inhalation is not suitable for treating the bronchial tubes.
Prof. Dr Fischer: Yes, PEP systems are helpful because they mechanically mobilise the mucus and keep the bronchial tubes open. PEP systems are especially helpful in patients with bronchial collapse – when the airways collapse when you breathe out, which means the mucus can no longer be transported out of the lungs. The vibrations generated by the PARI O-PEP are especially helpful at loosening mucus.
Prof. Dr Fischer: It can happen with either of these diseases. Many patients with bronchiectasis also have COPD, in which case their bronchial tubes are narrowed and also have dilations. There are also patients with bronchiectasis and normal lung function – but that is less common.
Prof. Dr Fischer: Yes, if the sputum turns from pale yellow to dark green, this indicates a bacterial infection. Reddish sputum or coughing up blood are also warning signs. It is essential that you see a doctor without delay. Generally, they will then perform a computer tomography of your lungs to identify the causes and to determine an effective treatment.
Prof. Dr Fischer: To prevent mucus production in cases of COPD and bronchiectasis, it is important to properly stick to the long-term therapy. It is also important to strictly avoid smoking – and that includes passive smoking – and to avoid exposure to fine dust, such as caused by open fires, woodburning stoves or busy roads.
It is also worth identifying any potential allergies, as these can also promote mucus production. Otherwise, mucus production is unfortunately a chronic problem requiring ongoing symptomatic treatment with measures to loosen the mucus such as inhalation therapy and respiratory physiotherapy.
Prof. Dr Fischer: We generally recommend doing inhalation therapy twice a day. This can be upped to three times a day if you have an infection or are producing more mucus than usual, for example in cough and cold season or if you have a viral infection. The frequency should be individually adjusted: If you do not have a buildup of secretions, you can do the inhalation therapy less often. More frequent inhalation therapy is not going to do any harm but it does take up more time. Respiratory therapy with PEP systems and the use of breathing techniques such as autogenic drainage or the pursed lips technique can also help better mobilise the mucus.
Prof. Dr Fischer:
Prof. Dr Rainald Fischer is a specialist for internal medicine in private practice, with a subspecialty in lung and bronchial medicine, specialty of emergency medicine, sleep medicine and allergy medicine in Munich-Pasing. Before that he worked as an internist and lung specialist, most recently as a senior physician at the Munich university hospital. Prof Dr Rainald Fischer is a founding member and president of the Deutschen Gesellschaft für Berg- und Expeditionsmedizin (German Society for Mountain and Expedition Medicine), and also a member of the Cystic Fibrosis Medical Association.
Note: The information in this blog post is not a treatment recommendation. The needs of patients vary greatly from person to person. The treatment approaches presented should be viewed only as examples. PARI recommends that patients always consult with their physician or physiotherapist first.